The spectre of antibiotic resistance looms large, threatening to send us back to a pre-antibiotic era where even minor infections could turn deadly. While the development of new antibiotics remains crucial, there’s a powerful weapon we often overlook in this fight: vaccines.

Beyond Prevention: Vaccines and the Collateral Benefit
Vaccines are traditionally seen as shields against specific infectious diseases. But their impact extends far beyond direct prevention. Here’s how vaccines act as a powerful indirect weapon against antibiotic resistance:
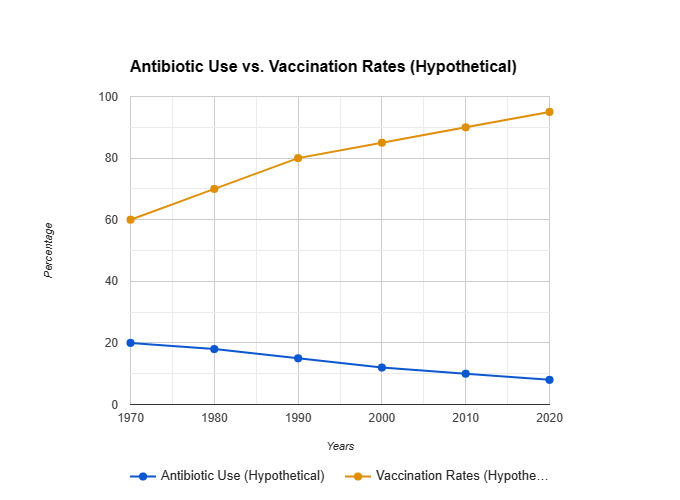
- Reduced Antibiotic Use: By preventing infections, vaccines significantly decrease the need for antibiotics in the first place. This reduces the selective pressure that drives the emergence of resistant bacteria. Imagine a battlefield – fewer antibiotics used means fewer opportunities for bacteria to develop resistance.
- Herd Immunity: When a high percentage of the population is vaccinated, it creates herd immunity, protecting even those who aren’t vaccinated. This reduces the overall circulation of the targeted pathogen, further limiting the spread of resistant strains.
- Boosting the Immune System: Certain vaccines, like those for pneumococcus and Haemophilus influenzae type b (Hib), can also strengthen the immune system’s overall response to infections. This can potentially reduce the severity and duration of infections, leading to less reliance on antibiotics.
Vaccines We Already Have, Weapons We Can Wield
The good news is that we already have a powerful arsenal of vaccines that can indirectly contribute to the fight against antibiotic resistance. Here are some key examples:


- Childhood Vaccinations: Routine childhood vaccinations for diseases like measles, mumps, rubella, diphtheria, tetanus, pertussis (whooping cough), and pneumococcus significantly reduce the need for antibiotics to treat these illnesses.
- Pneumococcal Vaccine: This vaccine protects against various strains of pneumococcus, a bacterium responsible for pneumonia, ear infections, and meningitis. By reducing pneumococcal infections, it helps curb the use of antibiotics for these conditions.
- Haemophilus influenzae type b (Hib) Vaccine: This vaccine protects against Hib, a bacterium that can cause meningitis, pneumonia, and epiglottitis (swelling of the upper airway). Vaccination has significantly reduced Hib infections, leading to a decrease in antibiotic use for these serious illnesses.
- Rotavirus Vaccine: This vaccine protects against rotavirus, a major cause of severe diarrhoea in children. By preventing rotavirus infections, it reduces the need for antibiotics often prescribed for diarrhoea.
A Timeline of Vaccines and Reduced Antibiotic Use
Here’s a glimpse into the historical impact of vaccines on antibiotic use:
- 1796: Edward Jenner develops the first vaccine – the smallpox vaccine. While antibiotics wouldn’t be discovered for another century, this pioneering work paved the way for future vaccines and their impact on overall infection rates.
- 1920s: The development of vaccines for diphtheria, tetanus, and pertussis leads to a significant decline in these bacterial infections, lowering the need for antibiotics to treat them.
- 1940s: The discovery of penicillin revolutionizes medicine, but concerns about overuse and resistance emerged early on. Vaccines like the one for Haemophilus influenzae type b (Hib), introduced in the 1980s, offer a crucial alternative for preventing Hib infections, and reducing pressure on antibiotic use.
- 1970s & 1980s: Pneumococcal conjugate vaccines are developed, targeting specific strains of this bacterium responsible for pneumonia, ear infections, and meningitis. These vaccines contribute to a decline in these infections and a decrease in antibiotic use for such conditions.
- 2000s & Beyond: The introduction of the rotavirus vaccine helps reduce the incidence of severe diarrhea in children, a condition often treated with antibiotics. Continued research explores next-generation vaccines targeting specific drug-resistant bacteria and broad-spectrum vaccines for a wider range of infections.
Your Role in the Fight
While large-scale research and development efforts drive vaccine innovation, individuals also play a crucial role:
- Stay Vaccinated: Ensure you and your family are up-to-date on recommended vaccinations. This simple act helps reduce the need for antibiotics and protects vulnerable populations.
- Spread Awareness: Educate others about the importance of vaccination and the indirect benefit it has in combating antibiotic resistance.
- Advocate for Research: Support organizations dedicated to vaccine research and development.
Frequently Asked Questions (FAQs) about Vaccines and Antibiotic Resistance
1. Is it safe to get vaccinated if I have allergies?
In most cases, yes. It’s important to discuss any allergies you have with your doctor before getting vaccinated. They can review your medical history and advise you on the appropriate course of action. Some vaccines may not be recommended for people with severe allergies to specific ingredients.
2. Can vaccines cause autism?
Extensive research has conclusively shown no link between vaccines and autism. This myth originated from a now-retracted study that has been thoroughly debunked by the scientific community.
3. Why do I need vaccinations if I’m healthy?
Vaccines not only protect you from getting sick, but they also help protect those around you, especially vulnerable populations like newborns, the elderly, and immunocompromised individuals. Vaccination creates herd immunity, meaning that even those who are not vaccinated have a lower risk of getting infected if enough people in the community are vaccinated.
4. What does antibiotic resistance have to do with vaccines?
Vaccines prevent infections, thereby reducing the need for antibiotics. This helps to slow down the development of antibiotic-resistant bacteria. When antibiotics are used less frequently, bacteria have fewer opportunities to develop resistance mechanisms.
5. Are there any side effects from vaccines?
Vaccines are generally very safe. Some people may experience mild side effects like soreness at the injection site, low-grade fever, or fatigue. These side effects are usually temporary and resolve on their own within a day or two.
6. Where can I get more information about vaccines and antibiotic resistance?
Here are some credible sources for further information:
- World Health Organization (WHO): https://www.who.int/health-topics/vaccines-and-immunization
- Centres for Disease Control and Prevention (CDC): https://www.cdc.gov/vaccines/index.html
- CDC Antibiotic Resistance: https://www.cdc.gov/drugresistance/index.html
7. What can I do to help combat antibiotic resistance?
There are several ways you can help:
- Get vaccinated and keep your vaccinations up-to-date.
- Only take antibiotics when prescribed by a doctor, and complete the full course of treatment even if you start feeling better.
- Never share antibiotics with others.
- Talk to your doctor about alternative treatments for minor illnesses that don’t require antibiotics.
- Spread awareness about the importance of vaccination and responsible antibiotic use.
By understanding the benefits of vaccines and taking action to prevent antibiotic misuse, we can all play a role in protecting ourselves and future generations from the growing threat of antibiotic resistance.
Vaccines are not just tools for individual protection; they are powerful allies in the global fight against antibiotic resistance. By promoting vaccination, we can minimize reliance on antibiotics, reduce the emergence of resistant strains, and secure a future where these life-saving medications remain effective. Together, through responsible vaccination practices and continued research, we can ensure that vaccines remain our first line of defense against a growing threat.