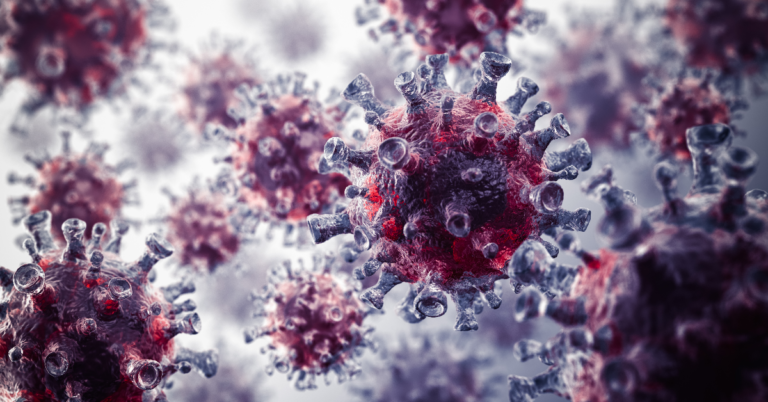
Antibiotics – those wonder drugs that revolutionized medicine – are facing a silent crisis. The rise of antibiotic resistance, where bacteria develop defences against these life-saving treatments, poses a significant threat to global health. While the economic burden of resistance is often quantified in billions, the true cost goes far beyond mere financial figures.
This article delves deeper, exploring the multifaceted economic impact of antibiotic resistance and its far-reaching consequences for individuals, healthcare systems, and society as a whole.
Antibiotics – those wonder drugs that revolutionized medicine – are facing a silent crisis. The rise of antibiotic resistance, where bacteria develop defences against these life-saving treatments, poses a significant threat to global health. While the economic burden of resistance is often quantified in billions, the true cost goes far beyond mere financial figures.

This article delves deeper, exploring the multifaceted economic impact of antibiotic resistance and its far-reaching consequences for individuals, healthcare systems, and society as a whole.
Beyond the Headlines: A Ripple Effect on Healthcare Costs
The immediate economic impact of antibiotic resistance lies in the increased cost of treating infections. When antibiotics fail, healthcare professionals are forced to:
- Resort to more expensive drugs: Newer, broader-spectrum antibiotics are often more costly than traditional ones.
- Extend hospital stays: Difficulty in controlling infections due to resistance leads to longer hospitalizations, driving up costs for both patients and healthcare institutions.
- Increased diagnostic testing: Identifying the right antibiotic for resistant infections requires more extensive and expensive diagnostic tests.
The Economic Burden of Antibiotic Resistance

Additional Diagnostic Test
Extended Hospital Stay


Use of Expensive Drug
The Human Cost: Productivity Losses and Lost Lives
The economic impact extends beyond hospital bills. Antibiotic resistance can lead to:
- Reduced workforce productivity: Individuals battling resistant infections experience prolonged illnesses, absenteeism, and potential long-term health complications, impacting their ability to work.
- Loss of income: Illness and extended hospital stays can lead to lost wages and financial strain on individuals and families.
- Increased mortality rates: Untreatable infections pose a significant mortality risk, with devastating consequences for families and a loss of human potential.
A Story of Resilience and Loss: Sarah’s Fight
Sarah, a vibrant young artist in her late twenties, fell ill with a seemingly routine urinary tract infection. Prescribed antibiotics, she initially felt improvement. However, the infection stubbornly returned, and tests revealed a strain of E. coli resistant to the first-line antibiotic. This news came with a heavy financial burden – a switch to a stronger antibiotic, additional tests, and a prolonged hospital stay. More importantly, it forced Sarah to put her freelance work on hold, jeopardizing her income and impacting her sense of independence. Sarah’s story is a stark reminder that antibiotic resistance isn’t just a healthcare statistic; it has a profound human cost.
A Beacon of Hope: Shining a Light on Solutions
While the threat of antibiotic resistance is significant, there are reasons to be optimistic. Here are some success stories that demonstrate the power of a multi-pronged approach:
- The Netherlands’ Antibiotic Stewardship Program: Implemented in the 1980s, this program reduced antibiotic use in animals by 70% over two decades. This decrease is directly correlated with a decline in antibiotic-resistant bacterial infections in humans.
- The Pew Charitable Trusts’ Combating Antibiotic Resistance Initiative: This initiative works to raise awareness, advocate for policy changes, and support research and development of new antibiotics. Their efforts are contributing to a global movement towards responsible antibiotic use.
- Pioneering Research in Phage Therapy: Phages, naturally occurring viruses that target specific bacteria, are being explored as a potential alternative to traditional antibiotics. Early research shows promise for treating antibiotic-resistant infections.
A Global Challenge:
The economic burden of antibiotic resistance is a global concern. Here’s where a multi-pronged approach is crucial:
- Antibiotic Stewardship: Promoting responsible use of antibiotics in human and animal medicine is vital to slow resistance development.
- Investing in Research & Development: Increased funding for research into new antibiotics and alternative treatment strategies like phage therapy is essential.
- Strengthening Surveillance: Robust global surveillance programs can track resistance patterns and inform treatment strategies.
- Public Awareness Campaigns: Educating the public on the importance of antibiotic stewardship and responsible medication use empowers individuals to play a role in combating resistance.
Beyond the Numbers:
The economic burden of antibiotic resistance paints a stark picture. It’s a story not just about rising costs, but about the human cost of lost productivity, potential disability, and even lives. By acknowledging the multifaceted nature of this threat and working together – researchers, healthcare professionals, policymakers, and the public – we can combat antibiotic resistance and safeguard our future health. The highlighted success stories offer a glimpse into the solutions that can make a difference.
References:
- World Health Organization (WHO): https://www.who.int/about
- Centres for Disease Control and Prevention (CDC): https://www.cdc.gov/
- The Pew Charitable Trusts: https://www.pewtrusts.org/en/

[…] Norovirus is a highly contagious virus that causes gastroenteritis, an inflammation of the stomach and intestines. Highlighting norovirus prevention and symptoms helps reduce the risk of infection in families. Overuse of antibiotics can lead to resistance, complicating treatments for bacterial infections that can follow viral illnesses. Learn more at The Silent Threat of Antibiotic Resistance. […]