Protecting Your Health with the Power of Prevention
Cervical cancer affects thousands of women every year, but there’s a powerful tool to prevent it: the HPV vaccine. This vaccine not only helps reduce the risk of cervical cancer but also protects against other cancers caused by the human papillomavirus (HPV).
While routine screenings such as Pap smears are critical in detecting cervical cancer early, prevention through vaccination has proven to be one of the most effective ways to combat this disease. In fact, since the introduction of the HPV vaccine, cervical cancer rates have significantly dropped in countries with high vaccination coverage.
In this article, we’ll explain how the HPV vaccine works, who should get it, and why it’s a critical step in protecting your long-term health.
What is HPV and Why Does It Matter?
HPV (Human Papillomavirus) is a group of over 100 viruses, some of which can lead to serious health issues, including cancer. Most people will get HPV at some point in their lives, but the majority of infections clear up on their own without causing harm. However, certain high-risk strains of HPV can persist and cause cervical, vaginal, vulvar, penile, anal, or throat cancers.
In the U.S. alone, around 14 million new HPV infections occur each year, with an estimated 10,000 new cases of cervical cancer. The good news is that the vaccine can protect against the most dangerous strains of HPV, significantly lowering the risk of developing these cancers.
Real-life Example:
Take the case of Australia, which implemented a nationwide HPV vaccination program in 2007. As a result, the country is now on track to eliminate cervical cancer as a public health problem within the next 20 years. Rates of HPV infection among vaccinated women have dropped by more than 90%, and the incidence of high-grade cervical abnormalities in young women has significantly decreased.
How Does the HPV Vaccine Work?
The vaccine works by triggering an immune response that helps the body fight off future infections from specific strains of HPV. There are currently three vaccines available:
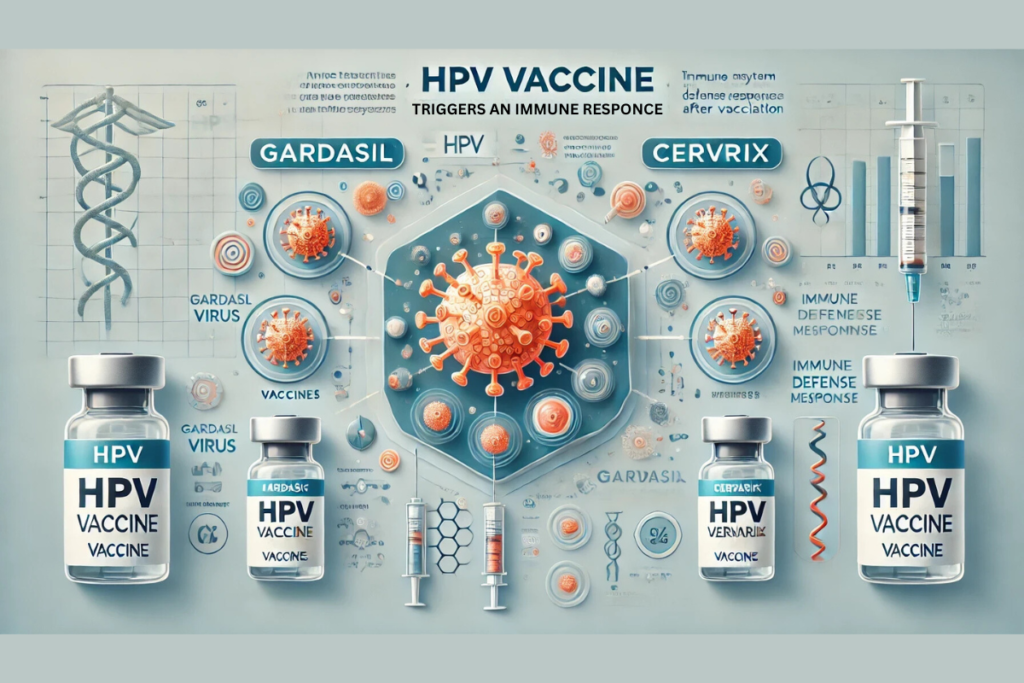
- Gardasil: Protects against HPV types 6, 11, 16, and 18, which cause the majority of cervical cancers and genital warts.
- Gardasil 9: Expands protection to cover five additional HPV types (31, 33, 45, 52, and 58).
- Cervarix: Protects against types 16 and 18, which are most strongly associated with cervical cancer.
Once vaccinated, the body develops immunity to these strains, making it much harder for HPV to cause an infection that could lead to cancer.
Check out the Gardasil vaccine information on WebMD for more details about the available vaccine options.
Who Should Be Vaccinated?
The vaccine is recommended for both girls and boys starting at ages 11 or 12, although it can be given as early as age 9. The reason for vaccinating at this age is that the vaccine works best when administered before any exposure to HPV, which is typically through sexual contact.
However, it’s not too late for older teens or young adults to get vaccinated. The CDC recommends vaccination for:
- Women up to age 26 who haven’t been fully vaccinated.
- Men up to age 21, although men up to age 26 who have sex with men or have weakened immune systems can also benefit from vaccination.
This vaccine is crucial because it protects against the strains most likely to cause cancer, even for individuals who may have already been exposed to other types of HPV.

Learn more about the HPV vaccine and cervical cancer prevention from the CDC.
Protecting Against Cervical Cancer Through Vaccination
Cervical cancer is one of the most common cancers among women worldwide, but it’s largely preventable thanks to the vaccine. According to the CDC, the vaccine is nearly 100% effective in preventing cervical cancers caused by HPV types 16 and 18.
In addition to cervical cancer, the vaccine protects against cancers of the vagina, vulva, anus, and oropharynx (throat). By getting vaccinated, women can significantly reduce their risk of developing these cancers. In fact, countries with high rates of HPV vaccination have seen dramatic decreases in cervical cancer cases.
Case Study:
A study conducted in Scotland found that women who were vaccinated before the age of 17 had a nearly 90% reduction in precancerous lesions compared to unvaccinated women. This reinforces the importance of early vaccination to maximize the preventive benefits.
In the U.S., routine screening with Pap smears and HPV testing also plays a key role in catching precancerous changes early, but the vaccine is the first line of defence. It works in combination with regular screening to provide the best protection against cervical cancer.
Read more
The Future of the HPV Vaccine: Expanded Uses and Innovations
The success of the HPV vaccine has sparked interest in using similar vaccine technology to fight other cancers and diseases. Researchers are exploring the possibility of developing vaccines against other cancer-causing viruses, such as hepatitis B and Epstein-Barr virus, which are linked to liver cancer and certain types of lymphoma.
There’s also ongoing research to make the vaccine more accessible worldwide. In some lower-income countries, access to vaccines is still limited, but global health initiatives are working to change that. Expanding access to the vaccine could save hundreds of thousands of lives annually by reducing cervical cancer rates worldwide.
Debunking Common Myths About the HPV Vaccine
Despite its effectiveness, there are still several myths about the vaccine that can prevent people from getting vaccinated. Let’s clear up some of the most common misconceptions.
- Myth 1: The vaccine is only for women.
Fact: The vaccine is recommended for both boys and girls because it prevents genital warts and cancer caused by HPV in both sexes. Men can also develop cancers from HPV, so it’s just as important for boys to be vaccinated. - Myth 2: The vaccine encourages risky sexual behavior.
Fact: Studies have shown that getting vaccinated does not influence sexual activity. The vaccine’s purpose is to protect against cancer, not regulate behavior. - Myth 3: The vaccine is only needed if you’re sexually active.
Fact: The vaccine works best when given before exposure to the virus, which is why it’s recommended for preteens. However, even sexually active individuals can benefit from the vaccine because it protects against multiple strains of HPV.
Safety and Side Effects of the HPV Vaccine
The HPV vaccine is extremely safe. Like any vaccine, it can cause mild side effects such as:
- Soreness at the injection site.
- Mild fever.
- Headache or fatigue.
Severe allergic reactions are very rare, and the benefits of vaccination far outweigh the risks. The vaccine has been rigorously tested in clinical trials and is recommended by major health organizations, including the CDC, WHO, and the American Cancer Society.
If you’re concerned about side effects, it’s important to know that most side effects are mild and go away on their own after a few days. Long-term safety data shows that the vaccine continues to be safe and effective for years after the initial dose.
Why You Should Get the HPV Vaccine
The HPV vaccine is a simple, safe, and highly effective way to protect yourself from a virus that can cause cancer. By getting vaccinated, you’re taking an important step toward safeguarding your health and the health of future generations.
Even if you’ve missed the recommended age range, it’s not too late to talk to your doctor about getting vaccinated. Whether you’re a parent thinking about your child’s future or an adult looking to protect yourself, the HPV vaccine offers powerful prevention against some of the most serious health risks.
Cervical cancer is a serious disease, but the HPV vaccine gives us the power to prevent it. With millions of doses safely administered around the world, the vaccine has already had a major impact on reducing HPV-related cancers. Don’t wait—if you or your loved ones haven’t been vaccinated yet, now is the time to take action.


[…] HPV Vaccine for Cervical Cancer Prevention […]
[…] HPV Vaccine for Cervical Cancer Prevention […]